Sports Safety / First Aid Clinic
Being a successful coach requires knowing more than just the skills and strategies of a sport. It includes being able to teach technique and tactics, motivate athletes and manage a myriad of details. It involves fulfilling the role of being a competent first responder to athletes injuries and illnesses.
Recognizing Emergencies
|
Unusual Noises
-Screams, yells, moans or calls for help -Breaking glass, crashing metal, screeching tire -Sudden, loud or unidentifiable sounds Unusual Sights -Stopped vehicle -Broken glass -Overturned pot in kitchen Unusual Odors -Odors that are stranger than usual -Unrecognizable odors -Inappropriate odors Unusual Appearance or Behavior -Unconsciousness -Confused or unusual behavior -Trouble breathing -Clutching chest or throat -Slurred, confused or hesitant speech |
Emergency Action Steps
First Aid
Give Immediate care to an athlete of injury or sudden illness until more advanced care can be obtained. A properly stocked first aid kit should include a pocket mask, scissors or a blade, bags for ice, medical history card for each athlete, and medical release forms.
Check
How do I evaluate (CHECK) an injured athlete?
How do I activate (CALL) the EMS?
How will first aid (CARE) be provided?
ABC's
Airway
Breathing
Circulation
Severe bleeding/shock
The primary concern when dealing with an injured athlete until professional help arrives are to activate an emergency plan, implement the ABC's and take precautions such as using gloves and face masks).
Emergency Action Plan
An emergency action plan should be reviewed by all responsible for caring for athletes.
If a cell phone is not available an effective action plan suggests that you should have enough change to make three or more pay phone calls.
Give Immediate care to an athlete of injury or sudden illness until more advanced care can be obtained. A properly stocked first aid kit should include a pocket mask, scissors or a blade, bags for ice, medical history card for each athlete, and medical release forms.
Check
How do I evaluate (CHECK) an injured athlete?
How do I activate (CALL) the EMS?
How will first aid (CARE) be provided?
ABC's
Airway
Breathing
Circulation
Severe bleeding/shock
The primary concern when dealing with an injured athlete until professional help arrives are to activate an emergency plan, implement the ABC's and take precautions such as using gloves and face masks).
Emergency Action Plan
An emergency action plan should be reviewed by all responsible for caring for athletes.
If a cell phone is not available an effective action plan suggests that you should have enough change to make three or more pay phone calls.
The Good Samaritan Law
In the United States
The details of Good Samaritan laws/acts in various jurisdictions vary, including who is protected from liability and in what circumstances. Not all jurisdictions provide protection to laypersons, in those cases only protecting trained personnel. In some cases, laypersons are only protected when rendering aid in narrow circumstances, such as during a declared public health emergency.
General Guidelines
Unless a caretaker relationship (such as a parent-child or doctor-patient relationship) exists prior to the illness or injury, or the "Good Samaritan" is responsible for the existence of the illness or injury, no person is required to give aid of any sort to a victim. Good Samaritan statutes in the states of Minnesota and Vermont do include a duty to assist subdivision requiring a person at the scene of an emergency to provide reasonable assistance to a person in need. This assistance may be to call 9-1-1. Violation of the duty to assist subdivision is a petty misdemeanor in Minnesota and may warrant a fine of up to $100 in Vermont. At least five other states including California and Nevada are considering duty to assist subdivisions of their Good Samaritan Statutes.
Any first aid provided must not be in exchange for any reward or financial compensation. As a result; medical professionals are typically not protected by Good Samaritan laws when performing first aid in connection with their employment.
If aid begins, the responder must not leave the scene until:
-It is necessary to call for needed medical assistance.
-Somebody of equal or higher ability can take over.
-Continuing to give aid is unsafe (this can be as simple as a lack of adequate protection against potential diseases, such as vinyl,
latex, or sterile gloves to protect against blood-borne pathogens) — a responder can never be forced to put himself or herself in danger to aid another person.
The responder is not legally liable for the death, disfigurement or disability of the victim as long as the responder acted rationally, in good faith, and in accordance with his level of training.
The details of Good Samaritan laws/acts in various jurisdictions vary, including who is protected from liability and in what circumstances. Not all jurisdictions provide protection to laypersons, in those cases only protecting trained personnel. In some cases, laypersons are only protected when rendering aid in narrow circumstances, such as during a declared public health emergency.
General Guidelines
Unless a caretaker relationship (such as a parent-child or doctor-patient relationship) exists prior to the illness or injury, or the "Good Samaritan" is responsible for the existence of the illness or injury, no person is required to give aid of any sort to a victim. Good Samaritan statutes in the states of Minnesota and Vermont do include a duty to assist subdivision requiring a person at the scene of an emergency to provide reasonable assistance to a person in need. This assistance may be to call 9-1-1. Violation of the duty to assist subdivision is a petty misdemeanor in Minnesota and may warrant a fine of up to $100 in Vermont. At least five other states including California and Nevada are considering duty to assist subdivisions of their Good Samaritan Statutes.
Any first aid provided must not be in exchange for any reward or financial compensation. As a result; medical professionals are typically not protected by Good Samaritan laws when performing first aid in connection with their employment.
If aid begins, the responder must not leave the scene until:
-It is necessary to call for needed medical assistance.
-Somebody of equal or higher ability can take over.
-Continuing to give aid is unsafe (this can be as simple as a lack of adequate protection against potential diseases, such as vinyl,
latex, or sterile gloves to protect against blood-borne pathogens) — a responder can never be forced to put himself or herself in danger to aid another person.
The responder is not legally liable for the death, disfigurement or disability of the victim as long as the responder acted rationally, in good faith, and in accordance with his level of training.
-Consent
The responder must not commit assault by giving aid to a patient without consent of the patient (or of the patient's legal parent or guardian if the patient is under 18 years old)
-Implied Consent
Consent may be implied if the patient is unconscious, delusional, intoxicated, deemed mentally unfit to make decisions regarding their safety, or if the responder had a reasonable belief that this was as such; courts tend to be very forgiving in adjudicating this, under the legal fiction that "peril invites rescue" (as in the rescue doctrine).
Consent may also be implied if the legal parent or guardian is not immediately reachable and the patient is not considered an adult.
Consent may also be implied if the legal parent or guardian is not immediately reachable and the patient is not considered an adult.
-Parental Consent
If the victim is not an adult (warning: definitions vary), consent must come from the legal parent or guardian. However, if the legal parent or guardian is absent, unconscious, delusional or intoxicated, consent is implied (with the same caveat as above). A responder may not withhold life-saving treatment (CPR, the Heimlich Maneuver) if the parent/guardian will not consent. The parent/guardian is then considered neglecting, and treatment is implied. Special circumstances may exist if child abuse is suspected.
-Laws for the first aiders only
In most jurisdictions, Good Samaritan laws only protect those that have had basic first aid training and are certified by the American Heart Association, American Red Cross, St. John Ambulance, American Safety and Health Institute or other health organization. In other jurisdictions, any rescuer is protected from liability, granted the responder acted rationally. If you are not trained in first aid or certified and perform first aid incorrectly you can still be held liable because you are not trained to perform first aid correctly.
Conscious Athlete
For a conscious athlete, one should always:
1) Ask questions such as: do you have allergies, are you taking any medications,
when did you last eat or drink, ask medical history.
2) Check the victim from head to toe.
3) Care for any conditions you find.
when did you last eat or drink, ask medical history.
2) Check the victim from head to toe.
3) Care for any conditions you find.
Secondary Survey
History, Inspection & Touch
HISTORY INSPECTION TOUCH
Injury Location Profuse bleeding Point tenderness
Whether a re-injury Skin appearance Skin temperature
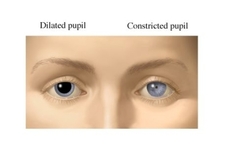
Injury mechanism Pupil size and reaction Sensation or numbness
Deformities Deformity
Swelling
Discoloration
Ability to walk
Moving Injured or Sick Athletes
Moving Critically Injured Athletes
Move only if you have to (i.e. scene is unsafe--in traffic, or to provide proper care). If you have to move use one person drag/rescue.
Moving Non-critically Injured Athletes
One person walking assist
Two person walking assist
Two handed seat carry
Shock
A condition in which the body fails to deliver oxygen to the vital organs, leaving the heart, lungs and brain with a lack of oxygen the body cannot function properly.
1) Place the victim in shock position by having the victim lay down.
2) Keep the person warm and comfortable.
Anaphylactic Shock: A severe allergic reaction to insect stings and spider bites, and certain food allergies.
Signs of Shock
MOOD: Restless or Irritable
PULSE: Fast or Weak
BREATHING: Fast or Shallow
SKIN: Pale, Cool or Moist
LEVEL of CONSCIOUSNESS: Drowsy or Unconsciousness
OTHERS: Nausea, Vomiting or Strong Thirst
Care For Shock
Call 9-1-1 immediatly!!
Control bleeding
Maintain normal body temperature
Position victim
No drink or food for victim
Moving Critically Injured Athletes
Move only if you have to (i.e. scene is unsafe--in traffic, or to provide proper care). If you have to move use one person drag/rescue.
Moving Non-critically Injured Athletes
One person walking assist
Two person walking assist
Two handed seat carry
Shock
A condition in which the body fails to deliver oxygen to the vital organs, leaving the heart, lungs and brain with a lack of oxygen the body cannot function properly.
1) Place the victim in shock position by having the victim lay down.
2) Keep the person warm and comfortable.
Anaphylactic Shock: A severe allergic reaction to insect stings and spider bites, and certain food allergies.
Signs of Shock
MOOD: Restless or Irritable
PULSE: Fast or Weak
BREATHING: Fast or Shallow
SKIN: Pale, Cool or Moist
LEVEL of CONSCIOUSNESS: Drowsy or Unconsciousness
OTHERS: Nausea, Vomiting or Strong Thirst
Care For Shock
Call 9-1-1 immediatly!!
Control bleeding
Maintain normal body temperature
Position victim
No drink or food for victim
Conscious Choking
Rescuer stands beside the choking person. Rescuer asks for permission to help and asks if the person is choking, then calls 9-1-1. Rescuer stands beside the person then reaches in front of the person crossing their arm across the person's chest grasping the opposite shoulder, leaning the person over. Administer five (5) back blows between the shoulder blades. If this does not work, rescuer stands the person straight up and places one foot between the person's feet. Rescuer reaches around the person placing one finger in the person's naval and wraps arm around the person, placing the flat side of hand, thumb side in, just above the finger that is in the naval. Then taking the hand that is in the naval out and placing it atop the hand that is thumb side in, administer five (5) abdominal thrusts in an upward motion.
Purpose: To dislodge an object causing total airway obstruction.
Bleeding

1) Add direct pressure.
2) Apply pressure bandage.
3) Apply additional pressure bandage.
4) For nose bleeds: Pinch nose lean head forward (preferably into a trash can or some other
receptacle ).
A sign of internal bleeding includes nausea and hardness of the abdomen to the touch.
To manage nose bleeds the following should be implemented: apply ice to the nose
area, pinch upper portion of the nose to apply direct pressure and have athlete stand with
head forward.
2) Apply pressure bandage.
3) Apply additional pressure bandage.
4) For nose bleeds: Pinch nose lean head forward (preferably into a trash can or some other
receptacle ).
A sign of internal bleeding includes nausea and hardness of the abdomen to the touch.
To manage nose bleeds the following should be implemented: apply ice to the nose
area, pinch upper portion of the nose to apply direct pressure and have athlete stand with
head forward.
Muscles, Bones and Joints

-Sprains
-Strains
-Dislocation (total disruption of
joint where bones are no longer in alignment)
-Fractures
Splint the injury only if transporting
-Do not attempt to reposition fractured or dislocated bones. This could sever nerves and arteries as well as cause further damage
to bones, ligaments, cartilage, muscles and tendons.
-Do not attempt to push exposed bones back under skin.
Sudden Illness
1) Life threatening care first
2) Help the victim rest
3) Maintain normal body temperature
4) Reassure the victim
5) Watch for changes
6) No food or drink unless fully conscious
Concussions1) A concussion is a brain injury.
2) All concussions are serious. 3) Concussions can occur without loss of consciousness. 4) Concussions can occur in any sport. 5) Recognition and proper management of concussions when they first occur can help prevent further injury or even deaths. A common indication of a head injury is slurred speech, ringing in the ears, and blurred vision. If you suspect a head injury have the athlete seen by a doctor. |
Diabetic Emergency - Condition in which an athlete's glucose (sugar) levels drop below normal levels (hypoglycemia). If this occurs the person needs to be given some form of sugar.
Seizures (convulsions)- Episode of abnormal electrical activity within the brain. It can lead to sudden changes in an athletes alertness, behavior, and muscle control.
When an athlete has a seizure, do not:
•Restrain the athlete
•Try to place anything in the athlete's mouth
•Try to pry teeth apart
After a seizure you should record the length of the seizure, assess the athlete's airway, breathing and circulation and transport them by EMS.
Seizures (convulsions)- Episode of abnormal electrical activity within the brain. It can lead to sudden changes in an athletes alertness, behavior, and muscle control.
When an athlete has a seizure, do not:
•Restrain the athlete
•Try to place anything in the athlete's mouth
•Try to pry teeth apart
After a seizure you should record the length of the seizure, assess the athlete's airway, breathing and circulation and transport them by EMS.
Asthma

A disease in which inflammation of the airways causes airflow into and out of
the lungs to be restricted.
You will recognize asthma when you see:
•Wheezing and difficulty breathing and speaking
•Dry, persistent cough
•Fear, anxiety
•Gray-blue skin
•Changing levels of responsiveness
Asthma can be triggered by allergies, exercise and rapid weather change.
In order to treat an athlete with asthma the following apply: reassure the athlete, have them take slow, deep breaths and remove any known environmental triggers or remove athlete from the area.
Another breathing issue, not to be confused with asthma, is hyperventilation, signs include: numbness, tingling in the hands and light headedness.
the lungs to be restricted.
You will recognize asthma when you see:
•Wheezing and difficulty breathing and speaking
•Dry, persistent cough
•Fear, anxiety
•Gray-blue skin
•Changing levels of responsiveness
Asthma can be triggered by allergies, exercise and rapid weather change.
In order to treat an athlete with asthma the following apply: reassure the athlete, have them take slow, deep breaths and remove any known environmental triggers or remove athlete from the area.
Another breathing issue, not to be confused with asthma, is hyperventilation, signs include: numbness, tingling in the hands and light headedness.
Heat and Cold Related Illnesses
|
Heat-Related Illnesses
Dehydration A condition caused by the athlete's loss of fluids from perspiration and prolonged exposure to heat and humidity. When the athlete's fluid loss exceeds his or her input through drinking, dehydration occurs and the blood volume lessens. A prolonged period of dehydration will lead to shock and in susceptible casualties, such as the frail and elderly and very young, can be fatal. Common signs of dehydration include: thirst, decreased performance and cramping. If a person experiences dehydration give 7-10 ounces of liquid every 10-20 minutes. Other heat related illnesses •Heat cramps •Heat exhaustion (exhibited in disorientation, profuse sweating, and a rapid weak pulse) •Heat stroke When any of these occur, cool athlete down with cool towels and water. Risk factors for heat illness include: dehydration, medications that cause dehydration and a history of illness. |
Cold-Related Illnesses
•Hypothermia •Frostbite -Do not rub or massage frostbitten areas. -Do not apply ice to frostbitten areas. -Do not allow frostbitten tissue to refreeze. |
Injury Prevention

Proper warm-up activities are essential in reducing injury, preparing an athlete's heart for physical exercise and allowing the athlete to rehearse movements and skills needed in the sport.
The cool down period allows for the body to return to its resting state. During a cool down period an athlete should stretch the major muscles or tight muscles.
During a stretch one should never bounce, but hold the stretch for 30 to 60 seconds.
If an injury does occur, ice is the primary remedy in order to reduce swelling, pain, and muscle spasms.
If an athlete displays blurred or loss of vision, ringing in the ears or swelling, they should not return to play until seen by a physician or other medical professional who can clear them for participation.
The cool down period allows for the body to return to its resting state. During a cool down period an athlete should stretch the major muscles or tight muscles.
During a stretch one should never bounce, but hold the stretch for 30 to 60 seconds.
If an injury does occur, ice is the primary remedy in order to reduce swelling, pain, and muscle spasms.
If an athlete displays blurred or loss of vision, ringing in the ears or swelling, they should not return to play until seen by a physician or other medical professional who can clear them for participation.
Ready to take the test?
Please read the instructions below.
Please read the instructions below.
You are about to take take a test to be certified through the Positive Sport Coaching Program.
While taking this test:
-If an error occurs use the "back" or "refresh" button to allow for the questions to proceed.
-The password for the test is Sports Safety/First Aid
-You must answer each question, even if it may not be correct. Don't worry, you are able to take it twice.
-An e-mail will be sent to you with upon passing and a certificate of completion
-Good luck and enjoy gaining knowledge on how you can be a Positive Sport Coach!
While taking this test:
-If an error occurs use the "back" or "refresh" button to allow for the questions to proceed.
-The password for the test is Sports Safety/First Aid
-You must answer each question, even if it may not be correct. Don't worry, you are able to take it twice.
-An e-mail will be sent to you with upon passing and a certificate of completion
-Good luck and enjoy gaining knowledge on how you can be a Positive Sport Coach!